Module 3
How to Participate
To participate in this training module, complete the following activities in the prescribed order:
- Complete the Pre-Test
- Read the training materials
- Complete the Post-Test

Learning Objective
At the end of this module, learners should be able to:
- outline infection prevention and control measures during COVID-19 vaccination sessions to protect health workers, vaccine recipients, and the community;
- describe how you prepare for vaccination sessions according to infection prevention and control protocols (at the health facility, for outreach, and for a campaign); and
- outline the process of safe administration of the COVID-19 vaccine and waste disposal
Importance of infection prevention and control
Infection prevention and control is a scientific approach with practical solutions designed to prevent harm caused by infection to patients and health workers and, as we have seen in the context of COVID-19, it is also quite relevant in the community during a pandemic. It is grounded in infectious diseases, epidemiology, social science, and health system strengthening. IPC occupies a unique position in the field of patient safety and quality universal health coverage, since it is relevant to health workers and patients at every single healthcare encounter. Proper adherence to standard infection prevention and control practices can:
- Protect you, as a health worker
- Protect your patients and clients, and
- Protect your family and the community.
Standard infection prevention and control strategies for vaccination sessions
There is now a WHO IPC aide memoire document which provides a summary of the standard infection prevention and control measures which are required for COVID-19 vaccination sessions. These are the standard recommended infection control measures for delivery of vaccines:
- Hand hygiene with alcohol-based hand rub or clean water and soap.
- Perform respiratory hygiene/cough etiquette.
- PPE: wear a medical mask
- Apply safe injection practices and safe disposal of waste
- Environmental cleaning and disinfection: maintain a clean environment, especially high-touch surfaces (e.g. chairs, tables, door handles).
Each of these measures are detailed below.
Hand Hygiene
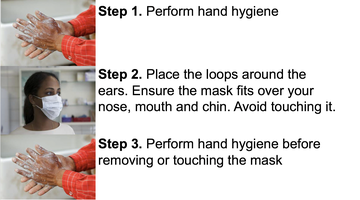
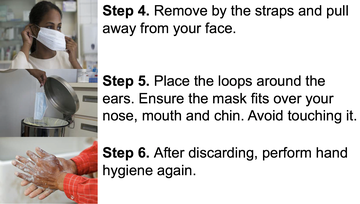
Vaccinators should always perform hand hygiene, preferably using alcohol-based hand rubs given their setting:
- before putting on and removing PPE (e.g. mask),
- before preparing the vaccine (especially when multi-dose vials are used), and
- between each person/vaccine administration.

Gloves are NOT indicated for intramuscular injections unless there is skin breakdown.
- If used, they do not replace the need for performing hand hygiene between each vaccine administration and for other indications.
- Applying alcohol-based hand rubs on gloved hands is strongly discouraged.
Personal protective equipment (PPE) items – masks
The type of PPE used will vary based on the health service provided, the individual risk assessment, and additional transmissionbased precautions needed. For delivering COVID-19 vaccines, the following PPE is recommended:
- medical masks – for the health worker; and
- medical or fabric mask for the person receiving the vaccine.
Ensure you are wearing a medical mask throughout the entire vaccination session. Refer to the image below for guidance on how to wear a mask.
Preparing for the Session
It is most important to inform the community and target groups in advance of the location and time for vaccination sessions. This is important that they know when to come, and they come to the right place at the right time. It is important to set up safe vaccination sites and ensure adequate quantities of:
- vaccines and supplies
- adequate cold-chain equipment
- appropriate injection equipment
- appropriate PPE
- safety boxes
- reporting tools.
Setting up vaccination sites
Follow these measures when setting up a vaccination site:

- Ventilation Ensure adequate (mechanical, natural or combination of both) ventilation. For natural ventilation, open windows and doors in indoor spaces. If outdoors, pick a well-ventilated area. For a mechanical ventilation system, the ventilation rate should be at least 6 air changes per hour. The recommended air exchange will depend on the setting and context. For further advice refer to national or international heating, refrigerating and air-conditioning regulation.
- Physical Distancing Ensure at least 1 meter distance in all directions between each person.
- Hand Hygiene Make available hand-washing stations or alcohol-based hand rub dispensers.
- Screening Screen for respiratory symptoms before those getting vaccinated enter the vaccination site.
- Crowd Control Limit the number of individuals to avoid crowding and long waiting times.
- Flow Ensure one-way flow through the vaccination site.
- Positioning Avoid positioning yourself face-to-face with the vaccine recipient. Position the patient sideways.
- Environmental Cleaning It has been seen that the virus that causes COVID-19 can survive in the environment on surfaces from hours up to days. Therefore, high standards of environmental cleaning and disinfection are important control measures. It is recommended that cleaning should be undertaken at least twice a day paying special attention to frequent high-touch surfaces such as door handles, tables, phones, and light switches.
Immunization Clinic Flow
Let us now look at the immunization clinic flow in detail. It is proposed flow, however, you might need changing depending on your context. Let us look at the diagram from the perspective of someone coming in for COVID-19 vaccination.
- **Eligibility Screening Area ** Ensures that the person falls in the group of those targeted for COVID-19 vaccination. If eligible, proceed to next step. ⬇
- Clinic Entrance ⬇
- Waiting Area It is important that people maintain proper physical distance at all times in the waiting area. ⬇
- **Registration / Q&A / Form Completion Area (multiple stations) ** when called, the person should go to the registration area where specific forms can be completed.⬇
- Medical screening / treatment area (as needed) Where the person should be screened for respiratory symptoms. If there are symptoms, the person should be immediately referred for treatment. Here, the person can also be checked for any contraindications for vaccination. ⬇
- Vaccination Area (multiple stations) Here, the health workers should provide COVID-19 vaccination using proper infection prevention and control measures as mentioned in the previous slides.⬇
- **Post Vaccination Waiting Area ** the person should be observed for at least 15 to 30 minutes for an AEFI.⬇
- Clinic Exit
Requirements for a vaccination session (fixed post)
- Vaccine doses = target number x adequate wastage factor (WF)
- Vaccine vials = vaccine doses ÷ X (number of doses per vial)
- Auto disable (AD) syringes: 1 per vaccine dose
- Diluents (if applicable): 1 per vaccine vial
- Reconstitution syringes (if needed): 1 per vaccine vial
- Safety boxes = total number of syringes ÷ 100
- Tally sheets (or other reporting forms, depending on recommendation, including tracking for 2 doses)
- List with contact phone numbers (e.g. supervisor, focal person for adverse events following immunization (AEFI), ambulance driver)
- AEFI kit and AEFI reporting forms (these are specific for COVID-19 vaccine)
- Infection prevention and control kit
- Waste bin/bag
Requirements for outreach or campaign vaccination session
Requirements for outreach or campaign vaccination sessions are similar to what's needed in fixed posts.
- Number of vaccine doses adjusted for wastage factor: target number x WF
- Number of AD syringes, diluents, reconstitution syringes and safety boxes adjusted for number of required vaccine doses
- Microplan of the area
- A vaccine carrier in good condition with coolant packs and foam pad
- Infection prevention and control kit
- Tally sheets (or other reporting forms, depending on recommendation, including tracking for 2 doses)
- List with contact phone numbers (e.g. supervisor, local AEFI focal person, ambulance driver), AEFI kit and AEFI reporting forms (specific for COVID-19 vaccine)
Recommended infection prevention and control kit for outreach/campaign
In addition to vaccination supplies, health workers are advised to carry IPC kits with them as a precaution. This kit contains PPE that may be required based on individual risk assessment. Eye protection, gowns, and gloves are not routinely required as they should be used only if dealing with suspected COVID-19 patients. Gowns and gloves should be discarded after single use.
Contents of infection prevention and control kit
This kit should, at minimum, contain products for hand hygiene, which includes: soap, clean water or veronica buckets (if sinks are not available), disposable or clean towels or alcohol-based hand rub products. As well as medical masks, eye protection, gloves, gowns, a waste bin or garbage bag.
Other useful items to consider: tissues, thermo-scans for screening, cleaning equipment, visual reminders/signage, physical barriers (to aid spatial separation).
7 Steps to Safe Injections
Here are the seven steps to giving safe injections. It is important that anyone giving injections follows these steps.
- Have a clean workspace
- Practice hand hygiene
- Using sterile safety-engineered (auto-disabled -AD) syringe
- Using sterile vial of vaccine and diluent
- Cleaning the skin
- Appropriate collection of sharps waste
- Appropriate waste management
Administration of intramuscular (IM) injection
Most COVID-19 vaccine presentations will require intramuscular injection. To give the injection,
- Perform hand hygiene between each vaccine administration.
- Hold the AD syringe barrel with fingers and thumb on the sides of the barrel and with the bevel of the needle facing upwards.
- Gently stretch and support the skin with the other hand and quickly push the needle at a 90° angle down through the skin into the muscle.
- Depress the plunger smoothly, do not move the needle under the skin.
- Pull the needle out quickly and smoothly at the same angle as it went in.
- Discard the needle and syringe straight into the safety box.
Safe waste disposal at health facility and in outreach/campaign
Waste disposal at health facility and in outreach campaign settings is essential. It is important to:
- Drop the used AD syringe needle end down into a safety box immediately after use.
- Never recap the needle.
- When the safety box is full (¾ of the box), keep in a secure place until final disposal.
- Dispose of empty vaccine vials and other waste in a separate container or a waste bag.
- Contaminated PPE is infectious waste and should be disposed of in a separate container or a waste bag as all other hazardous waste.
Closing the vaccination site
Closing the vaccination site is an integral part of holding a vaccination session and should be done properly. When closing this session,
- Discard in a separate waste bag or container any used reconstituted COVID-19 vaccine vials.
- Count the unopened COVID-19 vaccine vials and diluents and write down the number on the tally sheet.
- If in outreach/campaign, return unopened COVID-19 vaccine vials and diluents, the vaccine carrier, and coolant-packs to the distribution point.
- Calculate on the tally sheet the number of COVID-19 vaccines administered, number of vials received, opened, discarded, and returned and submit the tally sheet to the 1st level supervisor.
Summary of Key Points
- Respect standard infection prevention and control precautions for vaccination sessions, regardless of delivery strategy.
- Administer intramuscular (IM) injection vaccine in the arm (site).
- Safely dispose of sharps and other infectious waste.
Additional Resources
- Immunization in Practice (2015 Update)
- The WHO Field Guide for planning and implementing high-quality supplementary immunization activities (SIA)
- Immunization in the Context of COVID-19 pandemic (May 2020)
- Infection Prevention and Control Core Documents
- Infection Prevention & Control COVID-19 Technical Guidance Documents
- OpenWHO IPC Channel – with additional trainings
- Mask use in the context of COVID-19
- WHO guide to local production – WHO recommended handrub formulations
Average Rating: ☆ ☆ ☆ ☆ ☆ (0 reviews)




